A team of scientists from the National University of Singapore (NUS) has succeeded in developing a wireless technology to assist in photodynamic therapy (PDT) for cancer patients. This breakthrough will ensure light therapy can be carried out in inner body parts, which was not possible before.
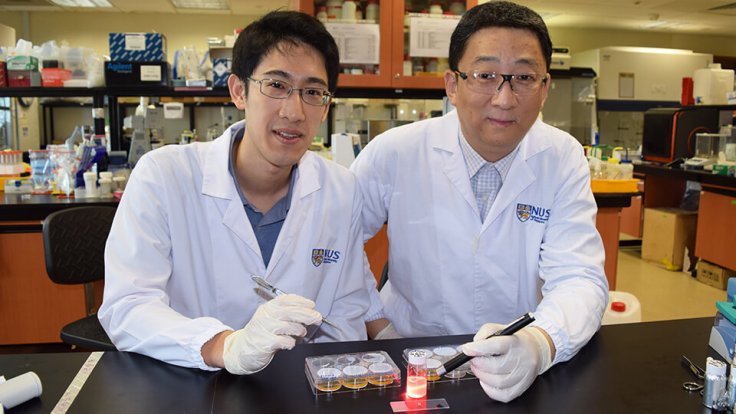
The study, supported by the Singapore Ministry of Education's Tier 3 grant, was led by Professor Zhang Yong from the Department of Biomedical Engineering and Assistant Professor John Ho from the Department of Electrical and Computer Engineering at NUS' Faculty of Engineering. Findings were published in the journal Proceedings of the National Academy of Sciences (PNAS) on January 29, 2018.
The use of wireless technology in PDT will make it suitable to treat a number of cancers, including brain and liver cancer. With the help of light delivery in deep regions of the body, tumour growth can be suppressed effectively.
The new research has found a way to deliver and control light in parts of the body, which will activate light-sensitive drugs for the therapy.
"This could potentially enable the therapies to be tailored by the clinician during the course of treatment," said Ho, who is also a Principal Investigator at the Biomedical Institute for Global Health Research and Technology (BIGHEART) at NUS.
Also read: Less traffic and quick travel make us happier than sex, says study
What is photodynamic therapy?
Photodynamic therapy or PDT is a cancer treatment method which makes use of light-sensitive drugs called photosensitizers. These drugs are triggered by a specific wavelength of light and produce a form of oxygen to kill nearby cells.
It can be used for targeted cancer treatment that is devoid of whole-body side effects incurred by traditional cancer treatments like chemotherapy.
PDT also shrinks and destroys tumours by damaging its blood vessels and cutting nutrient supply to them. It also activates the immune system to fight against cancers.
Limitations of the treatment
Although PDT is highly effective, it has so far been used only to cure surface cancers, like skin cancer, as it is difficult to make the light penetrate body tissues to reach deeper regions.
Organs at a depth of less than a centimeter from the surface are best suited for this treatment method using LEDs and lasers. Inner linings of organs, like oesophagus, can be reached by inserting a thin, lighted tube to view the affected tissues. However, organs like the brain and liver can only be reached by PDT after they are exposed to surgery.
New development
The team at NUS has achieved light penetration into deeper organs by inserting a tiny needle wireless device that reaches the target site. The device, which has 30 mg weight and 15 mm3 size, is easy to implant and has a special radio-frequency system that wirelessly powers the device and regulates the amount of light reaching the organ.
The effectiveness of this therapy was demonstrated by activating photosensitizers through tissues more than three centimeters thick. Multiple controlled light doses were applied to suppress tumour growth in these regions.
"This novel approach enables ongoing treatment to prevent reoccurrence of cancer, without additional surgery. The application of the technology can also be extended to many other light-based therapies, such as photothermal therapy, that face the common problem of limited penetration depth. We hope to bring these capabilities from bench to beside to provide new opportunities to shine light on human diseases," said Zhang.
Further research
The team is now focusing on the development of nanosystems that will deliver photosensitizers to targeted sites. They are also hopeful to inventing minimally invasive techniques to implant the devices in the body and integrating the sensors to the device to achieve real-time monitoring of treatment response.









