While scientists from all over the world are still in the process of understanding the pathogen of novel Coronavirus, researchers from Columbia University Irving Medical Center explained in their new study that one of the human immune system's oldest branches—'Complement system' also known as complement cascade—which acts as a part of the innate immune system can work with the adaptive immune system, if necessary, may be influencing the severity of COVID-19 disease.
As per the Columbia University researchers, people with age-related macular degeneration—a health condition caused by an overactive complement that leads to severe or permanent vision loss in elderly people-- are at greater risk of developing severe complications and dying from COVID-19.
The Research on Complement System
The new study, which was published in Nature Medicine, said that the connection with complement has suggested that existing drugs that inhibit the complement system could help treat patients with severe disease.
The Columbia University researchers also found evidence that clotting activity is linked to COVID-19 severity and that mutations in certain complement, as well as coagulation genes, are associated with hospitalization of patients with SARS-CoV-2.

Sagi Shapira, who led the new study along with Nicholas Tatonetti, both professors at Columbia University Vagelos College of Physicians and Surgeons said that together these results have given an important insight into the pathophysiology of novel Coronavirus and "paint a picture for the role of complement and coagulation pathways in determining clinical outcomes of patients infected with SARS-CoV-2."
Shapira said viruses have proteins that can mimic some host proteins to trick the host's cells into aiding the virus with completing its life cycle. "Based on our previous work and the work of others, we suspected that identifying those mimics could provide clues about how viruses cause disease," he noted.
As explained by the experts, the Coronavirus is the master of mimicry, mostly with proteins involved in coagulation and proteins that make up the complement system, which works like antibodies and helps to fight pathogens. This one of the oldest branches of the immune system can also increase coagulation and inflammation in the body.
Shapira said, "The new coronavirus -- by mimicking complement or coagulation proteins -- might drive both systems into a hyperactive state."
Rising the Risk
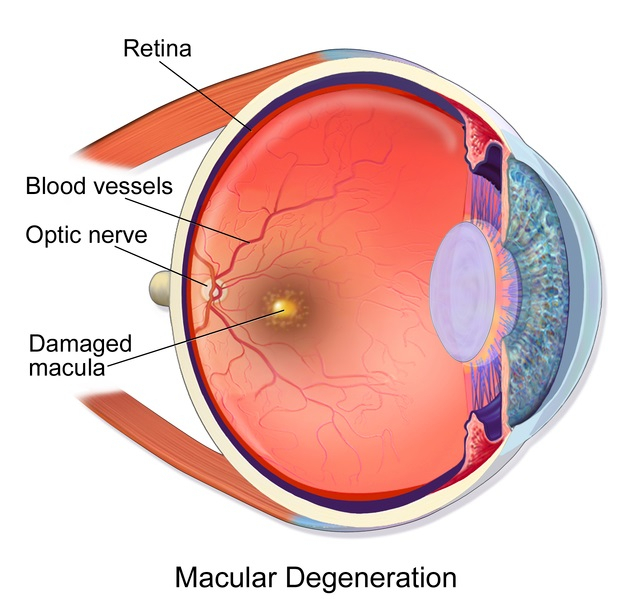
If the coagulation and complement system influence the severity of the novel Coronavirus, people with pre-existing hyperactive complement or coagulation disorders could be more susceptible to the virus. This idea led the researchers to look at the COVID-19 patients with macular degeneration as well as common coagulation disorders like thrombosis and hemorrhage.
The study said around 11,000 patients visited the Columbia University Irving Medical Center with suspected COVID-19 and later 6,398 tested positive for the disease. As the researchers said in the study, they identified 88 patients with a history of macular degeneration, four with complement deficiency disorders, and 1,179 with coagulatory disorders. "We observed a 35 percent mortality rate among patients that were put on mechanical ventilation and that 31 percent of deceased patients had been on mechanical respiration," wrote authors.
Shapira said complement is also more active in obesity and diabetes, and she believes that it may help to explain, why people with those conditions also have a greater mortality risk from Coronavirus. The researcher also added that even though these variants are not necessarily going to determine the outcome, the recent finding is another line of evidence that "complement and coagulation pathways participate in the morbidity and mortality associated with COVID-19."









