Turning to existing drugs to counter the onslaught of COVID-19 is gaining increasing prevalence. Now, a study by an international team of researchers has found that baricitinib, a drug used to treat rheumatoid arthritis (RA), can significantly reduce mortality in patients suffering from the SARS-CoV-2 coronavirus infection.
According to scientists, baricitinib can not only block the entry of the virus but also reduce deaths in hospitalized COVID-19 patients by two-thirds. The same research team had stated in a previous study that it had leveraged artificial intelligence (AI) to identify the drug as a potential candidate to treat the disease.
"We are pleased to report a 71 percent reduction in mortality for the group receiving baricitinib in addition to standard care. These results are especially encouraging seeing as the study included a large cohort of elderly patients, a group that is often excluded in other trials," said Dr. Volker Lauschke, corresponding author of the study, in a statement.
Picked By AI As A Potential Drug

Baricitinib is most commonly sold under the brand name Olumiant and is prescribed to adults who suffer from moderate to severe forms of the RA. It is specifically given to adults whose condition cannot be controlled using RA drugs known as tumor necrosis factor (TNF) antagonists. Baricitinib may be used individually or in combination with other drugs to treat the disease.
In February 2020, the same team of scientists from the Imperial College London and the Karolinska Institutet, Sweden, turned to an AI algorithm to identify a potential drug candidate from amongst thousands for repurposing against the novel coronavirus. The algorithm led to the identification baricitinib as a likely candidate to treat COVID-19.
Reducing Death Rates Drastically
As a part of the study, 83 patients (median age of 81) who were hospitalized in Spain and Italy with COVID-19, received baricitinib along with standard care. It was found that there was a 71 percent reduced risk of dying in patients who were treated using the drug in comparison to those who were not. The authors also discovered that only 17 percent of patients who received baricitinib succumbed to the disease or required mechanical ventilation, as against the 35 percent in the control group who did not receive the drug.
Baricitinib was found to be generally well-tolerated and aided in the decrease of inflammation from the beginning of the treatment. Side-effects associated with long-term use of the drug such as coagulopathy and thrombosis were not noted among the patients, probably due to treatment with anti-coagulation medication.
Some adverse effects such as bacterial infections and cardiovascular and gastrointestinal complications were observed. However, these effects were also found in the control group; raising doubts about any link to baricitinib.
"The study suggests this drug can aid recovery of patients with moderate to severe COVID-19, and may provide a new weapon in our arsenal against the virus. Large-scale clinical trials of this drug, to further investigate its potential, are now under way," said Dr. Justin Stebbing, co-lead author of the study.
Blocking the Entry of Virus
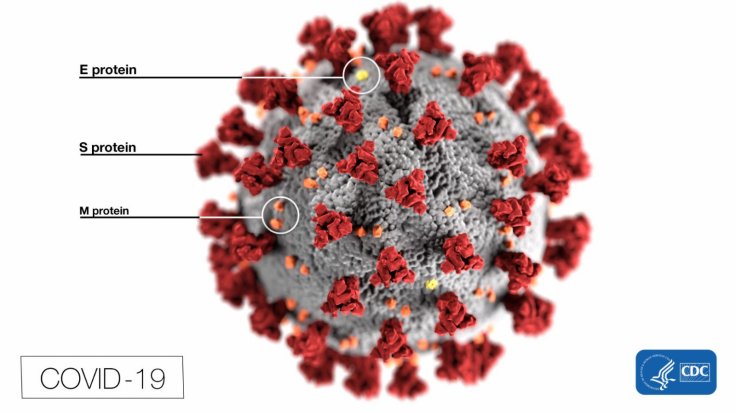
Cytokines are signaling proteins that regulate the immune system by drawing immune cells to the site of infection. However, in patients suffering from severe COVID-19, the signaling mechanism of the immune system is affected and a turbulent response known as a 'cytokine storm' damages healthy cells. Also, these "storms" increase the prevalence of ACE2 receptors—an enzyme that the SARS-CoV-2 uses to gain entry into human cells.
The researchers demonstrated that interferon, a cytokine, increases the availability of receptors, or 'docking points' for the coronavirus to bind with. They illustrated that the drug effectively blocks the entry of the virus into cells by eliminating "docking points" for the virus.
Studies have shown that COVID-19 enhances the activity of genes associated with platelets, which makes the blood more adhesive and increases the likeliness of clots forming. Baricitinib, however, was found to decrease the action of these genes. The authors also used organoids of human liver cells, RNA sequencing and super-resolution microscopy, and ascertained that the damage caused to liver cells was different from those in the cells of pulmonary organs.









