The role of antibodies in the recovery as well as treatment of COVID-19 has been a prime topic of research for scientists studying the deadly SARS-CoV-2 coronavirus. A new study by researchers from the Massachusetts General Hospital has found that the evolution of antibody (IgG) responses in an infected individual dictate the outcome of the disease in them.
According to the study, individuals in whose bodies the antibody response did not evolve or develop fully, most often did not survive the disease. However, patients in whom there was an evolved response had a positive prognosis.
"There was a significant defect in the development of IgG antibodies, which may be essential in the early control and elimination of the virus. Here, we were able to see the global impact of this defective IgG evolution, resulting in a compromised ability to promote essential viral clearing immune functions," said Dr. Galit Alter, lead author of the study, in a statement.
Comparing Antibody Responses
Several studies have described who produces what kind of antibodies and which of these are the most effective in helping the individual recover as well as serve as ideal candidates for plasma donation. The current study, however, focused on the idea that the quality and not quantity decided who survived COVID-19 and who did not.
For the study, the authors analyzed the early evolution of antibody response in 193 hospitalized COVID-19 patients. Using the serological profile obtained, the scientists compared the antibody immune responses with patients with moderate-to-severe forms of the disease and patients who succumbed to the infection.
Evolution of Antibodies
Though all the patients with COVID-19 developed antibodies against the novel coronavirus, the manner in which the antibodies evolved or developed, differed greatly among the three groups. A mature immune response is characterized by antibodies that both guide the immune system to destroy infected cells and block the infection.
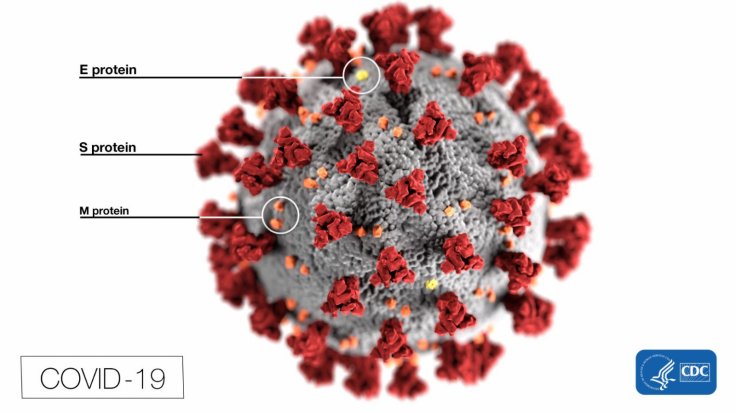
In order to direct the killer immune responses, the antibodies bind to a receptor known as 'Fc-receptor', which is specific to antibodies that are found on all immune cells. In the absence of a strong Fc-receptor binding, antibodies could fail to latch on to the virus and destroy them in the event of an infection.
The authors learnt that in comparison to survivors, patients who died of the disease possessed antibodies that had not fully 'evolved' the capacity to bin strongly with Fc-receptors. Hence, they may have lacked the ability to initiate immune killing activity fully.
Role of Pre-existing Immunity

Additionally, the researchers are also discovered that the immune systems of the survivors could identify and attack the 'S2 domain', an area on the of the SARS-CoV-2 spike protein—an structure that the virus uses to invade human cells. It is important to note that the S2 domain is found in other virulent coronaviruses that can infect humans. Therefore, it is possible that the antibodies may have been able to target the area due to pre-existing immunity acquired by exposure to the S2 domain of the viruses such as the common cold.
The scientists also posited that patients who antibodies that could recognize S2 domains on multiple coronaviruses, may potentially be able to mobilize this pre-existing immunity to produce killer antibodies more quickly after contracting the SARS-CoV-2 infection.
"If we can further understand the importance of cross-coronavirus immunity, researchers may be able to design vaccines able to counteract a much broader range of coronaviruses," concluded Tomer Zohar, lead author of the study.









