Anti-retroviral therapy has enabled individuals with human immunodeficiency virus (HIV) infection to live healthier lives and prolonged their life expectancy. Alas, some of the damage caused by the virus is lasting, including central nervous system damage. A new study states that the brains of patients with HIV suffer from an inability to effectively process sound.
The study, which is a collaboration between researchers from Dartmouth's Geisel School of Medicine and the Auditory Neuroscience Laboratory at Northwestern University, has demonstrated that the brain's auditory system is impaired due to the infection. "Initially, we thought we'd find that HIV affects the ear, but what seems to be affected is the brain's ability to process sound," said Jay Buckey, Jr, co-lead author of the study, in a statement.
Employing A Non-Invasive Method of Assessment
In order to test their hypothesis, the authors employed a technique known as a speech-evoked frequency-following response (FFR). The study involved 68 HIV-positive patients and 59 HIV-negative adults from Dar es Salaam, Tanzania.

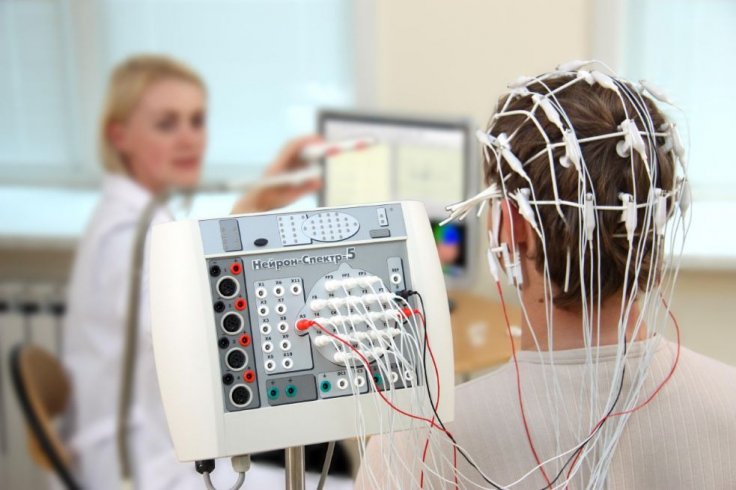
Using FFR, the brain waves of the participants are recorded using an electroencephalogram (EEG) while common sounds associated with everyday speech such as ba, da and ga played into their ears. The advantage of this method is that it does not require any invasive procedures to record brain waves of the individuals and analyze the auditory functions of their brains.
Nina Kraus, co-lead author of the study, explained that everyday speech is a mixture of key acoustic elements such as pitch, harmonics, timing, and phrase. She added: "The FFR enables us to play speech sounds into the ear of study participants and figure out how good a job the brain is doing processing these different acoustic ingredients."
Disruption In Responses of The Brain
After recording the FFR readings of both groups, the scientists compared their results. They found that in HIV-positive adults, the auditory-neurophysiological responses to specific speech cues were distorted. This was despite the fact that they performed in hearing tests. Therefore, the difference in the responses confirmed their hypothesis that the hearing difficulties faced by them were rooted in the central nervous system.
Highlighting the intricacy of the auditory process and the role of FFR in understanding it, Kraus illustrated, "When the brain processes sound, it's not like a volume knob where all of the acoustic ingredients are either processed well or poorly. With the FFR, we're able to see which aspects of auditory processing are affected or diminished and ask, 'Is there a specific neural signature that aligns itself with HIV?'"
A Viable Tool
According to the researchers, FFR can serve as a feasible tool not only for studying the complexities of brain dysfunction in HIV-positive patients, but also other disorders where brain activity is affected. These ailments can include Alzheimer's disease, concussion, and the Zika virus infection.
Buckey further stressed that the assessment of cognitive functions requires individuals to complete tasks such as puzzles and mathematical problems. However, FFR eliminates the need for such an examination. "What's significant about our results is that the test doesn't require any actions on the patient's part; it's recorded passively--subjects can even sleep or watch a movie," asserted Buckey.









