The capacity of the SARS-CoV-2 virus to infect human cells with ease has baffled scientists since the onset of the COVID-19 pandemic. Over the course of 2020, it has been learnt the virus gains entry into human cells through the ACE2 receptors found on them. However, a new study states that the coronavirus is using another receptor known as Neuropilin-1 to infiltrate human.
According to the study by an international team of researchers, Neuropilin-1—which is found in abundance in human tissues such as neurons, respiratory tracts, and blood vessels, could be serving as the entity that leads the virus to cells.
"If you think of ACE2 as a door lock to enter the cell, then neuropilin-1 could be a factor that directs the virus to the door. ACE2 is expressed at very low levels in most cells. Thus, it is not easy for the virus to find doors to enter. Other factors such as neuropilin-1 might help the virus finding its door", said Dr. Giuseppe Balistreri, lead author of the study in a statement.
Unusually High Virulence of SARS-CoV-2
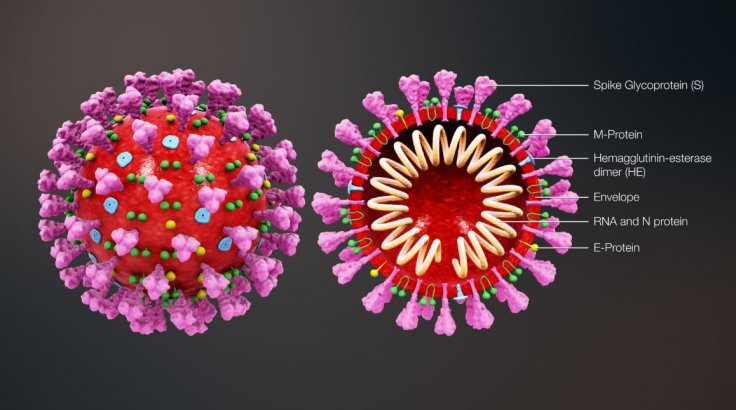
Studies have shown that the lethal novel coronavirus gains access to human cells by binding with angiotensin-converting enzyme 2 (ACE2) receptors. The virus uses its 'spike'—a hook-like protein structure found on its surface that it uses to latch on—to invade cells.
Also, the SARS-CoV-2 is closely related to the SARS-CoV that causes Severe Acute Respiratory Syndrome (SARS). SARS-CoV binds with ACE2 receptors as well. However, the significant difference between their virulence led the scientists to believe that there could be more to the COVID-19-causing pathogen's infection mechanism.
"That SARS-CoV-2 uses the receptor ACE2 to infect our cells was known, but viruses often use multiple factors to maximize their infectious potential," said Dr. Balistreri. In comparison to other respiratory viruses, it also infects the upper respiratory system including the nasal mucosa. Therefore, the study began with the premise that there was something different between SARS-CoV and SARS-CoV-2 despite the binding with the same receptors, expressed Ravi Ojha, co-author of the study.
Another Key Target to Attack Cells
In order to explain the difference, the international cohort of researchers examined the viral spike protein more closely. Dr. Balistreri averred that after the genome sequence of the SARS-CoV-2 was made available at the beginning of 2020, he found a particular aspect of the virus very fascinating.
"Compared to its older relative, the new coronavirus had acquired an 'extra piece' on its surface proteins, which is also found in the spikes of many devastating human viruses, including Ebola, HIV, and highly pathogenic strains of avian influenza, among others. We thought this could lead us to the answer," explained Dr. Balistreri.
The collaborative effort among the scientists led to a crucial discovery—the extra piece or key binds to neuropilin-1. Their experiments offered support for the floated hypothesis. Also, the results were consistent with another study by scientists from the University of Bristol, which had found that the virus' spike binds with neuropilin-1 directly. The two studies complement each other.
Taking The Nasal Route
The loss of smell is one of the primary symptoms of the coronavirus infection. Interestingly, neuropilin-1 is known to be found in the cell layer lining the nasal cavity. Therefore, the authors examined the tissue sample from patients who succumbed to the disease. "We wanted to find out whether cells equipped with neuropilin-1 are really infected by SARS-CoV-2, and found that this was the case," said Prof. Mika Simons, co-leader of the study.
Studies in mice provided evidence that suggested that that neuropilin-1 assists in transportation from the nasal mucosa to the central nervous system The mice were nasally administered tiny and virus-sized particles, that were chemically engineered nanoparticles designed to link to neuropilin-1. The scientists discovered that a few hours after administration, the nanoparticles made their way to the neurons and capillary vessels of the brain, while control particles with no affinity to neuropilin-1 did not.

"We could determine that neuropilin-1, at least under the conditions of our experiments, promotes transport into the brain, but we cannot make any conclusion whether this is also true for SARS-CoV-2. It is very likely that this pathway is suppressed by the immune system in most patients," explained Simons.
Potential for Development of New Therapeutics
Another interesting finding of the current study was that by blocking neuropilin-1 with antibodies, the authors were successfully able to reduce infection in laboratory cell cultures significantly. However, Dr. Balistreri cautioned that it was too premature to speculate whether directly blocking neuropilin-1 can be used as an effective therapeutic option, as it is not without the risk of side effects. Thus, further study is required to test its feasibility.
"Currently our laboratory is testing the effect of new molecules that we have specifically designed to interrupt the connection between the virus and neuropilin. Preliminary results are very promising and we hope to obtain validations in vivo in the near future," concluded Dr. Balistreri.









