In a development that can enable the formulation of improved treatments for patients suffering from cancer, researchers have created a modified version of an immune cell known as natural killer (NK) cells using stem cells to fight effectively against leukemia or blood cancer.
According to the study by researchers from the University of California San Diego School of Medicine, induced pluripotent stem cells (IPSCs) were used to create NK cells, from whom a gene called CISH was deleted. These 'super' NK cells were effective against tumors that are caused by leukemia, both in vivo and in vitro.
"These studies demonstrate that we can now edit iPSC-derived NK cells to remove an inhibitory gene inside the cell to improve activation of NK cells", said Dan Kaufman, senior author of the study.
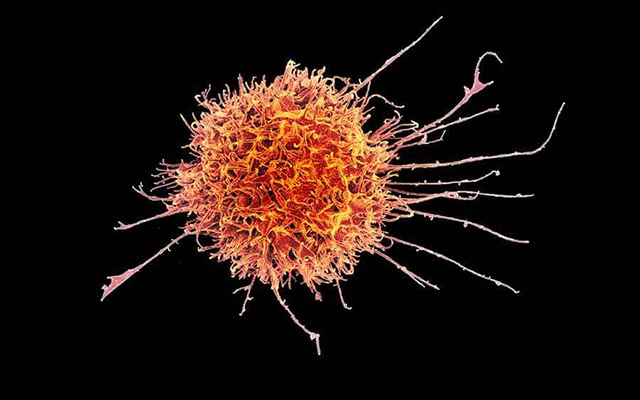
What Are Natural Killer (NK) Cells?
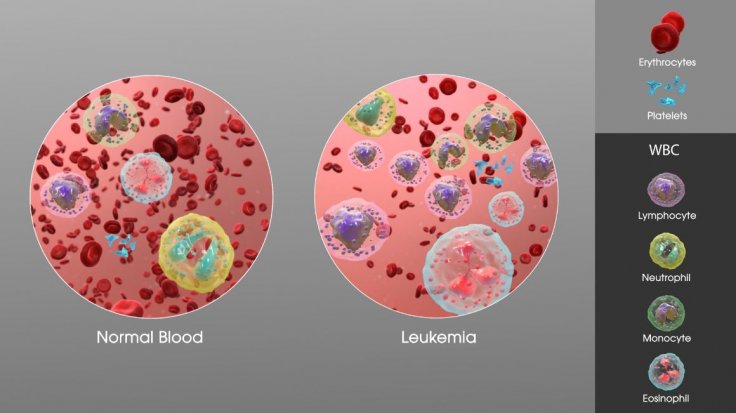
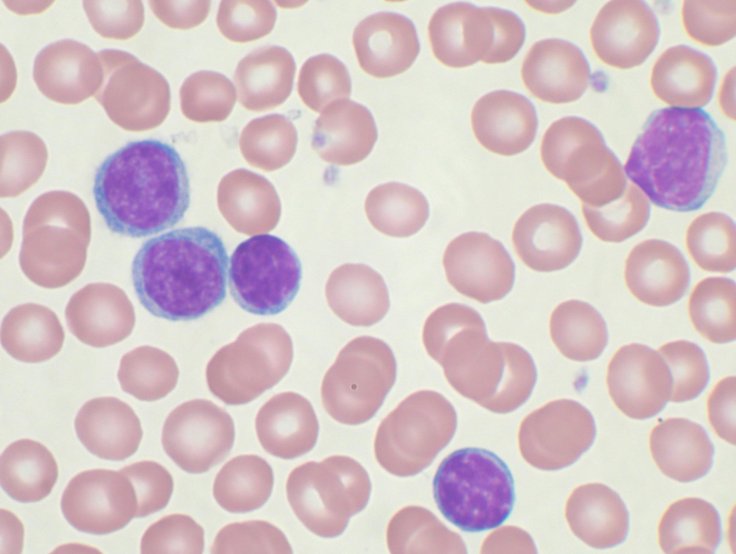
NK cells, also known as large granular lymphocytes (LGL) are lymphocytes—a type of white blood cells (WBCs)—that belong to the same class of WBCs such as T and B cells. They play an important role in the body's innate immune system, providing a rapid response to an infection.
These cells circulate across the body. In the presence of foreign or invading cells such as bacteria, virus, and even early cancer cells, they form the first immune response. With the ability to identify and target malignant cells, they hold great significance as the basis for therapies against cancer. However, their efficiency has been found to be limited. This where the newly created NK cells come into play.
Creating Modified NK Cells
The first step that the researchers carried out was the creation of modified NK cells for the study. They did this using IPSCs, which are harvested from blood or skin cells, after being reprogrammed to revert to an embryonic-like pluripotent state. Then they were designed to form NK cells. A benefit of this method is that it enables in the production of a standardized cell population as against the need to isolate cells for individual patients.
Next, the team eliminated a gene CISH from the newly created NK cells. The gene plays a key role in the expression of a molecule called the T-cell receptor (TCR), which suppresses the signaling of cytokines. The signaling proteins regulate the immune system by drawing immune cells such as fibroblasts, lymphocytes and macrophages to the sites of inflammation, infection and trauma.
Curing Leukemia In Mice
In order to test the effectiveness of the modified NK cells, the scientists treated mice that harbored human leukemia cells. While some mice were treated with the modified variant, the others were with regular NK cells. It was found that the altered NK cells effectively cured the mice treated with it. However, the mice treated with regular NK cells succumbed to leukemia.
"Deletion of CISH in NK cells removes an internal 'checkpoint' that is normally activated or expressed when NK cells are stimulated by cytokines, such as IL15," explained Kaufman. He illustrated that the deletion of the CISH gene in the iPSC-derived NK cells improved their activation.
It did so in two ways. First, it eliminated the inhibitory action on the cytokine Interleukin-15 or IL15. This significantly improved the activation and functioning of NK cells, even when the concentration of IL15 was low. Second, the NK cells became metabolically reprogrammed, which improved their efficiency.
Role In New Cancer Therapies
Kaufman expounded that iPSC-derived NK cells are already being used in clinical trials to treat hematologic (blood) malignancies as well as solid tumors. With the arrival of CISH-deleted iPSC-NK cells, these treatments can achieve larger efficacy.
"Importantly, iPSCs provide a stable platform for gene modification and since NK cells can be used as allogeneic cells that do not need to be matched to individual patients, we can create a line of appropriately modified iPSC-derived NK cells suitable for treating hundreds or thousands of patients as a standardized, 'off-the-shelf' therapy," he concluded.









