The race to find a drug that can help combat COVID-19 is on, with a few potential candidates offering a ray of hope emerging. Now a multi-institutional study has identified a new potential drug that may prevent or alleviate the consequences of the deadly SARS-CoV-2 infection.
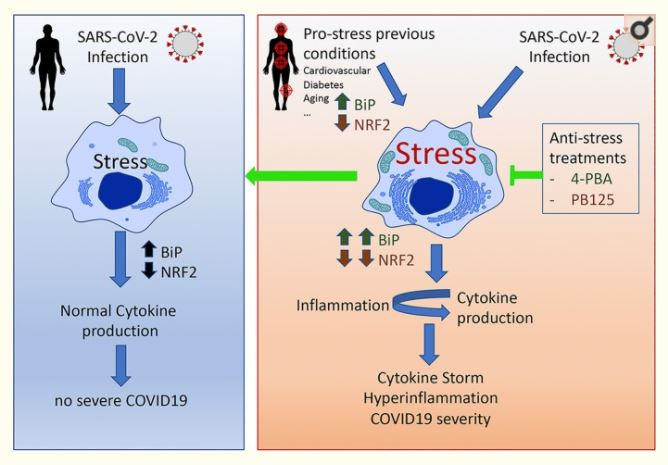
The research, a collaboration between scientists from the University of Malaga (UMA) and the Andalusian Centre for Nanomedicine and Biotechnology (BIONAND), focused on the modulatory effect of a compound known as 4-Phenylbutiric acid (4-PBA) on the haywire inflammatory response known as "Cytokine Storm" caused by severe COVID-19. Preliminary animal studies conducted by the team have shown positive results.
Mitigating Excessive Immune Response
One of the most lethal complications caused by the virus is an excessive inflammatory response—Cytokine storm. Cytokines are signaling proteins that moderate the immune system by attracting immune cells to the area of infection.
In patients with severe COVID-19, the signaling mechanism is impeded and an erratic response of the immune system or a 'cytokine storm', causes damage to healthy tissues. This leads to injury to the lungs and other vital organs, and eventually death. Currently, no prescribed treatment to mitigate this condition in COVID-19 patients exists.
It is this erratic immune response that researchers are trying to tackle with the new drug. "When cells are stressed by infection, they call the cytokines, and the more stressed they are, the more persistent they become, provoking this uncontrolled inflammation. Hence, one possible treatment for COVID-19 is to reduce cellular stress", explained Iván Durán, lead author of the study.
Repurposing a Clinically Approved Drug
4-PBA is a drug used to treat "urea cycle disorder", a metabolic disorder leading to excessive production of urea in the body. The drug has also shown anti-cancer properties in studies. According to the researchers, repurposing a clinically approved drug enables easier clinical application. It could regulate cellular stress, which is also found in other conditions such as diabetes, carcinogenesis or aging, which have been identified as risk factors for the novel coronavirus infection.
"Our preliminary results conducted on animal models have demonstrated that 4-PBA fully curbs mortality caused by respiratory failure derived from cellular stress," said Durán. He also illustrated that through their initial studies a protein known as "BiP" (Binding Immunoglobulin Protein)—a blood marker of stress— was identified. It serves as an indicator of cellular stress occurrences and may be examined and measured in patients with adverse COVID-19.
Identification of Risk Groups
According to Durán, the levels of BiP—along with the determination of the efficiency of 4-PBA therapy—may also help recognize COVID-19 risk groups. This can establish a correlation between high levels of BiP and the severity of inflammation after the contraction of the coronavirus infection.
"There are people already suffering from diseases that cause cellular stress, and when they become infected with coronavirus, they are more likely to fall ill or die. Therefore, if we know that the patient suffers from cellular stress, we can kill two birds with one stone: we can detect susceptibility before infection occurs and know how to treat it in due time," concluded Durán.









