It is a known fact that SARS-CoV-2 coronavirus, the cause behind the ongoing COVID-19 pandemic, can ravage the human body. However, it is said to have been harmless in bats (the supposed source) and the accepted intermediary host (pangolins) through which it made the jump to human beings. So what led to it acquiring its virulence? A new study states that numerous 'silent' mutations may have led to its ability to infect humans.
Researchers from Duke University spotted several 'silent' mutations in the approximately 30,000 letters of the pathogen's genetic code that lead to it flourishing in human beings after making the leap. According to the authors, the minute changes were associated with the manner in which the RNA molecules of the coronavirus were folded within human cells. "We're trying to figure out what made this virus so unique," said, Alejandro Berrio, lead author, in a statement.
Identifying Deadly Mutations
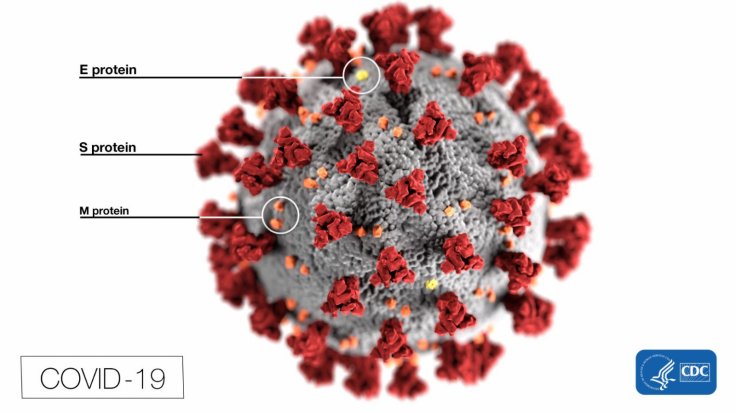
For the study, the researchers utilized statistical techniques that they designed to identify the adaptive changes that developed within the SARS-CoV-2 genome in humans, however, not found in closely related coronaviruses that are found in pangolins and bats. Previous studies have recognized distinctive impressions of positive selection in a gene that is linked to the encoding of the deadly spike protein—a structure used by the virus to invade human cells—found on its surface.
The current study found new mutations that transformed the spike proteins, thereby, proposing that strains of virus possessing these mutations had an increased likeliness of thriving. It also identified other culprits that were not detected by previous research.
'Silent' Mutations Arming the SARS-CoV-2 in Humans

According to the researchers, the 'silent' mutations—termed as Nsp4 and Nsp16—were found on two other regions of the COVID-19-causing pathogen's genome. They appear to have armed the SARS-CoV-2 the biological superiority over its predecessor strains without effecting any changes in the proteins encoded by them. Berrio stated that these changes may have had an effect on how the virus' RNA—its genetic material—folds into 3-D shapes and operates within human cells.
What the alterations in the RNA's structure could have done to lead to a clear distinction between the SARS-CoV-2 virus in human beings and other coronaviruses (the one's in bats and pangolins), remain unknown. However, the scientists agree that it most likely imbibed the virus with the ability to rapidly spread before people could recognize their infection status.
New Molecular Targets for Treating COVID-19
The discoveries made through the study may lead to the targeting of new molecular sites within the virus that can lead to the containment or treatment of COVID-19, highlighted Berro. "Nsp4 and Nsp16 are among the first RNA molecules that are produced when the virus infects a new person. The spike protein doesn't get expressed until later. So they could make a better therapeutic target because they appear earlier in the viral life cycle," he said.
In addition to understanding the underlying factors that led to the thriving of the novel coronavirus in human hosts, identifying its genetic changes may enable in better prediction of future deadly zoonotic disease outbreaks even before they can take hold.
"Viruses are constantly mutating and evolving. So it's possible that a new strain of coronavirus capable of infecting other animals may come along that also has the potential to spread to people, like SARS-CoV-2 did. We'll need to be able to recognize it and make efforts to contain it early," concluded Berrio.









