Oncologists often turn to immunotherapy to treat patients with cancers such as melanoma. However, its effectiveness can vary, with the results being close to nil in some individuals. However, researchers have now found that a drug that triggers the immune responses of the body by mimicking a virus can also make certain notoriously well-hidden melanoma tumors visible to the immune system. This may help immunotherapy in targeting melanoma cells better.
According to the study by scientists from the UCLA Jonsson Comprehensive Cancer Center, BO-112, a synthetic non-coding double-stranded RNA (dsRNA), can open new avenues in targeted immunotherapy by mimicking viruses. It may be able to do so by overcoming resistance to immunotherapy in tumors where the signaling of interferon—proteins released in the boy during an infection—is defective.
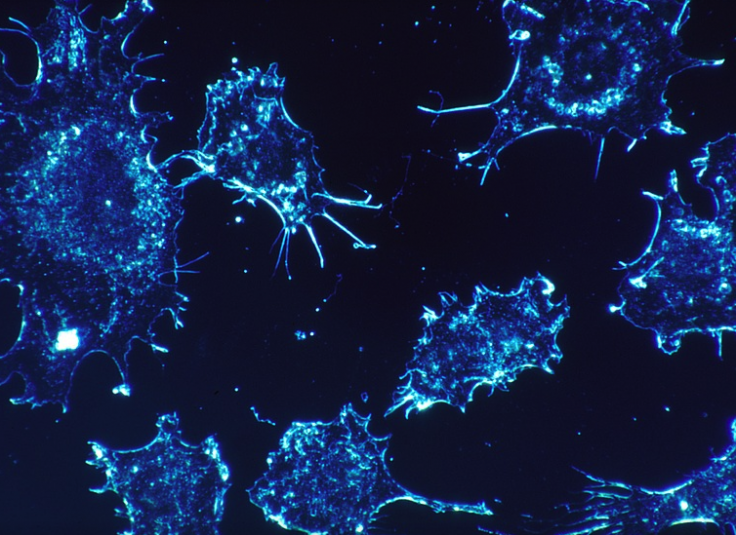
"Most immunotherapy approaches rely on the ability of T cells to recognize and kill tumor cells. But in some patients, tumors escape the immune system through mutations in genes involved in the interferon signaling pathway. This is a critical pathway because it normally allows tumors to increase their antigen presentation, an intricate machinery that makes tumors visible to T cells," said Dr. Anusha Kalbasi, lead author of the study, in a statement.
The Role of Interferons
Interferons are signaling proteins that are produced within the body and released by cells in response to viral infections. Infected cells also release interferons in order to alert the surrounding cells and heighten their ant-viral responses.
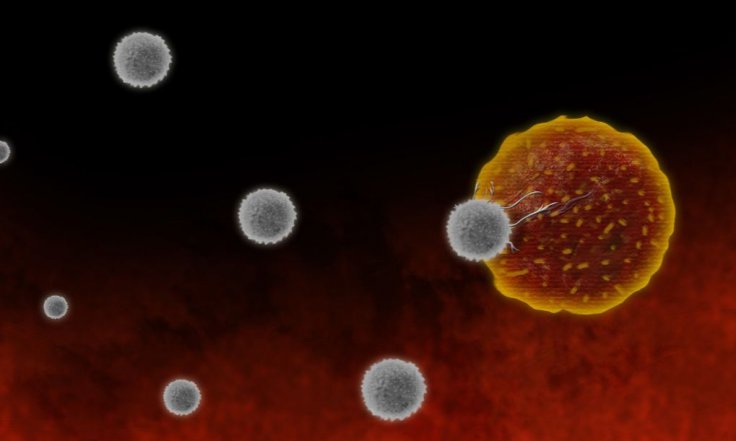
The activation of interferon signaling in tumors curbs the division of tumor cells and causes the release of molecules that attract more immune cells to the tumor. "This coordinated effort as a result of interferon signaling can help the immune system better identify and kill tumor cells," explained Kalbasi.
Engineering Melanoma Cells
First, the authors aimed to subdue defective signaling of interferons through adoptive T-cell therapy, which is a form of immunotherapy where lymphocytes known as T-cells are obtained from a patient and re-designed to identify and kill cancer cells. However, it was found that tumor cells with defective interferon signaling were not affected by T-cells.
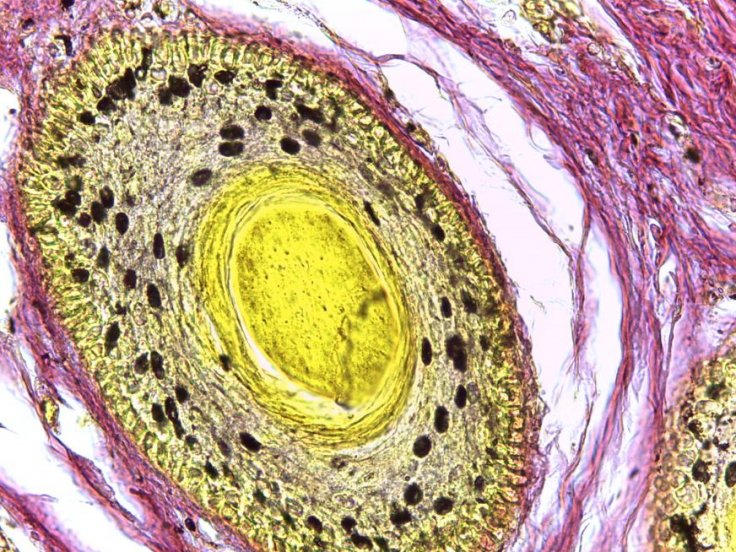
Next, the authors used a gene called NLRC5 to engineer melanoma tumor cells from mice. The gene was found to increase antigen presentation—a crucial immune process that vital for triggering the response of T-cells—even when interferon signaling was absent. It also re-established the efficacy of T-cells. Though the approach was successful in mice, it was not as simple to engineer human tumor cells.
Using Virus-mimicking Drug to Kill Cancer Cells
The research team resorted to the use of the virus-mimicking drug BO-112 that triggers in virus-sensing pathways within tumor cells. Upon injecting the drug directly into tumor cells under laboratory conditions, the authors found that the activation of the virus-sensing pathways ked to the increase of antigen presentation despite defective interferon signaling. Hence, the tumor cells were recognized and destroyed by T-cells.
"This study helps us understand the interdependence between interferon signaling and antigen presentation, which gives us important insights into how tumor cells are recognized by the immune system. New strategies to promote antigen presentation to make tumors more visible to the immune system will allow immunotherapy to be effective for even more tumor types," highlighted," said Dr. Antoni Ribas, senior author of the study.
Through the study, the scientists managed to emphasize the potential that other promising clinical approaches that bypass and antigen presentation and tumor interferon signaling hold. These include therapies such as chimeric antigen receptor-based T-cell therapy or CAR, that can identify and destroy tumor cells even when antigen presentation is absent.









